Group Activ Travel - UIN
ADITYA BIRLA HEALTH INSURANCE CO. LIMITED.
Group Activ Travel - Policy Terms and Conditions
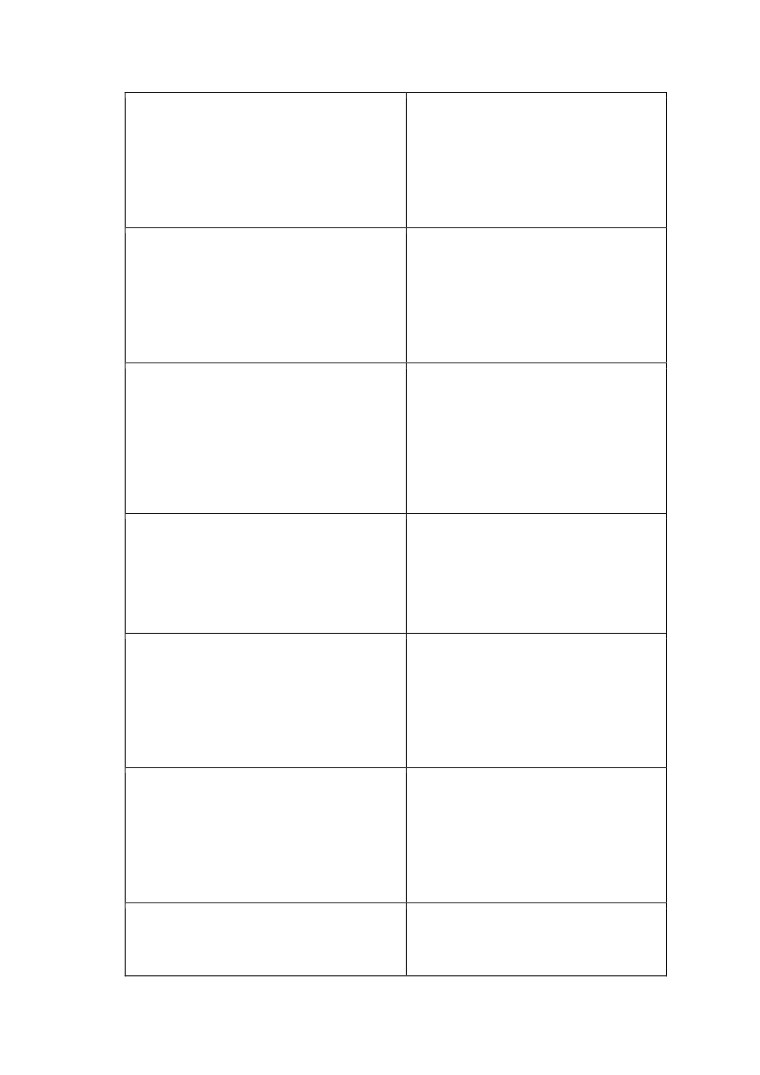
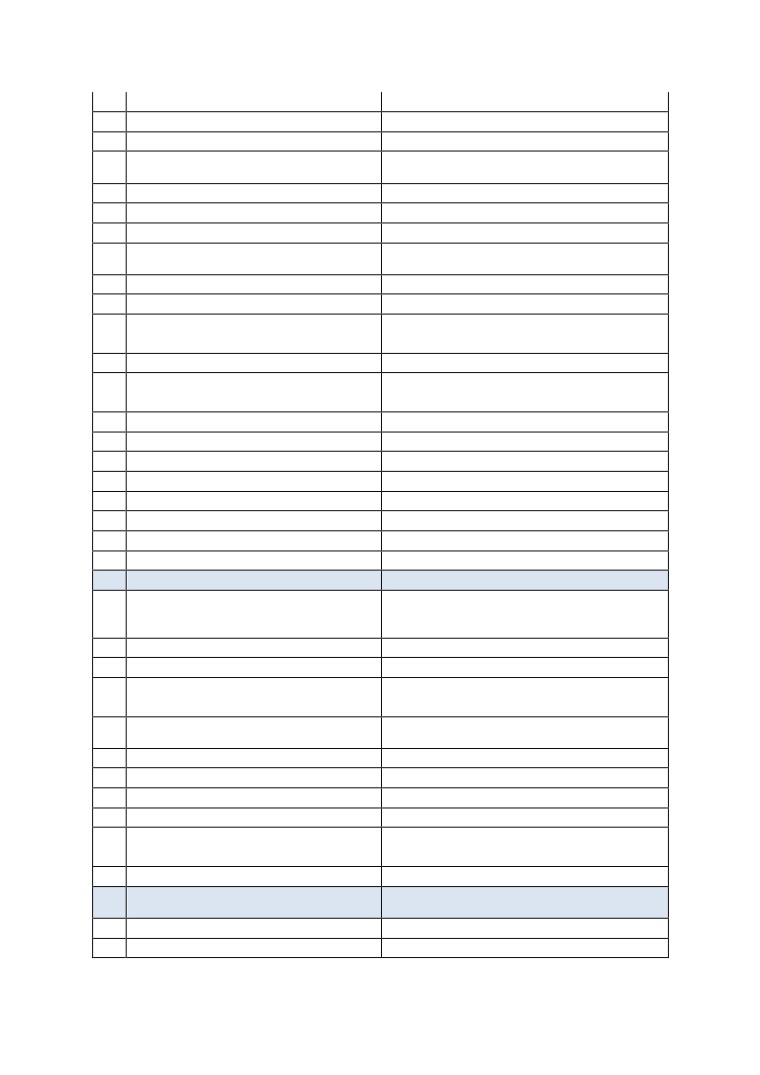
Policy Benefits
Coverage
Cover
Payout
Limit / Options
No.
Basis
In-patient Care
SI: Rs 2,00,000
1
with day care
Indemnity
Payout: Up to 100% of SI on In-patient hospitalisation with day
treatment
care treatment
COVERAGE DESCRIPTION
Sum insured
2 lakhs
16 days
Cover period
Both single trip and round trip are eligible to be covered under this trip. In case of round
trip, date of end of trip of last travel shall be considered as trip start date in this case.
Self only cover. Customer of Make my trip completi ng trip through ticket purchased using
Family definition
MakeMyTrip Travel portal / website, Applicable for air & hotel passengers only
Age band
3 months - 60 years
Initial waiting period
No
Room rent
At actuals.
Other costs related to
Cost of hospitalisation related treatment
treatment
Emergency Ambulance
Emergency Ambulance - up to 1% of S.I.
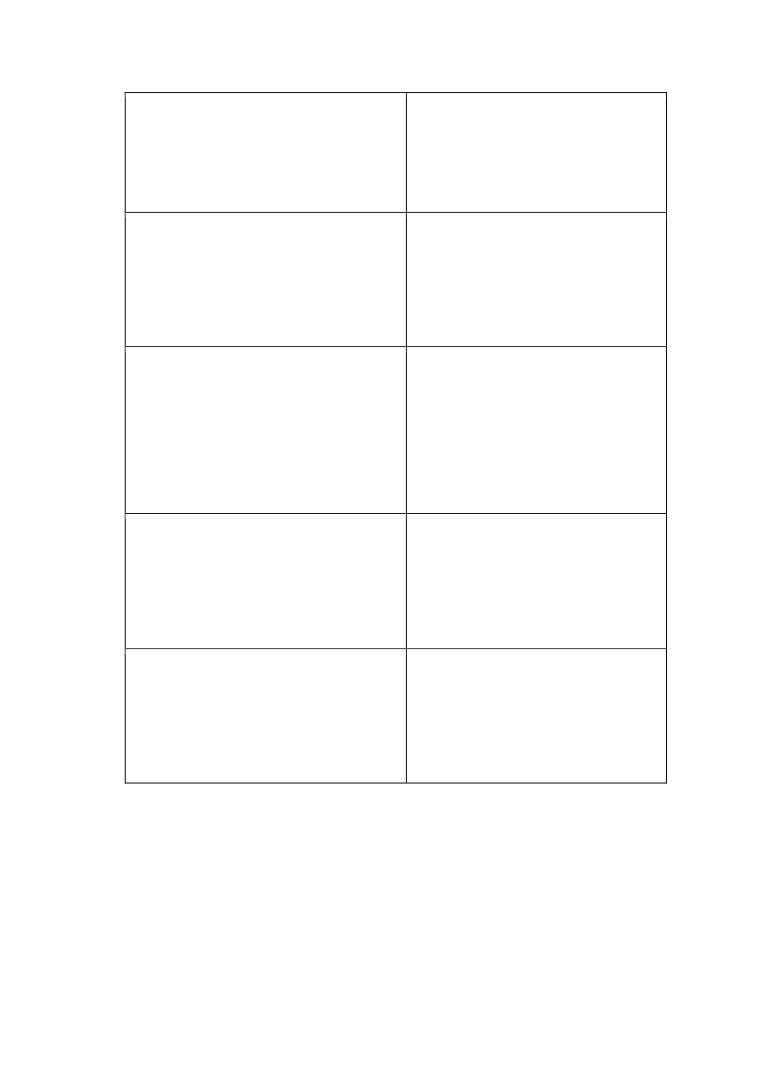
This Policy shall cover only Persons who meet all the below criteria:
• Indian residents & Citizens
• Persons aged between 3 months to 60 years.
• Persons who are not in Self Quarantine/Isolation, recommended
Quarantine/Isolation or already in Quarantine/Isolation at the time of Proposal.
Eligibility criteria
• Persons who are not Immunocompromised. Immunocompromised Persons
include Persons who have undergone Hospitalization, surgery or Day Care
procedure(s) within 90 days immediately preceding the Certificate Period Start Date.
• Persons who have not travelled to the travel -restricted countries specified by
the Central Government or Union Health Mini stry of India in 45 days immediately
preceding the Certificate Period Start Date.
•
Sub Limits are not applicable in the policy
•
In patient hospitalisation treatment with day care valid for emergency care.
Emergency Care means management for an illness or injury which results in
symptoms which occur suddenly and unexpectedly, and requires immediate care by a
medical practitioner to prevent death or serious long-term impairment of the insured
person’s health;
•
Policy Period means the period commencing from the Policy Period Start Date and
ending on the Policy Period End Date as specifically appearing in the Policy Schedule;
Condition
•
COVID-specific conditions:
o The Insured Person claiming this Benefit has a certificate from a Medical
Practitioner along with a Positive Virology Report from ICMR - National Institute
of Virology Pune, India or any other laboratory authorized by ICMR, confirming
the Insured Person(s) has been infected with COVID-19.
o Safety measures must be ensured by target customers as per government
advisory.
o Test has to be recommended by authorised medical practitioner as per clinical
protocol/guidelines issued by ICMR
Page 1 of 25
Group Activ Travel - UIN
• Treatment for pre-existing diseases/ conditions will not be covered
• Co-habitation: No claim shall be payable where the Insured Person was living with
and sharing the same address as that of person(s) who were Diagnosed with COVID-
19 or Quarantined at the time of Proposal.
Specific Exclusions:
• Unauthorized Testing center: Testing done at a Diagnostic center other than the ones
authorized by the Union Health Ministry of India. shall not be recognised under this
Policy.
• Out of India: Diagnosis and/or Treatment taken outside India is not covered.
• Self-Quarantine or Quarantine at home is not covered
Claim servicing
Claim service through in-house only.
Good health
Customer declaration for each passenger
declaration
Section A. PREAMBLE
This Policy has been issued on the basis of the Disclosure to Information Norm, including the information
provided by You in respect of the Insured Persons in the Proposal Form, any application for insurance cover in
respect of any Insured Person and any other information or details submitted in relation to the Proposal Form.
This Policy is a contract of insurance between You and Us which is subject to the receipt of premium in full and
accepted by Us in respect of the Insured Persons and the terms, conditions and exclusions as specified in the
Policy Schedule/Certificate of Insurance/Product Benefit Table of this Policy.
Key Notes:
The terms listed in Section D (Definitions) and which have been used elsewhere in the Policy shall have the
meaning set out against them in Section D (Definitions), wherever they appear in the Policy.
Section B. BENEFITS UNDER THE POLICY
Benefit B.1. “Medical Cover” is an in-built Benefit and is available to all Insured Persons. The Certificate of
Insurance will specify which of the Optional Benefits and Optional Extensions are in force for the Insu red
Person.
All Claims shall be payable subject to the terms, conditions and exclusions of the Policy and subject to
availability of the Sum Insured. Our maximum, total and cumulative liability in respect of an Insured Person
for any and all Claims arising under a Benefit/Optional Benefit during the Period of Insurance shall not exceed
the benefit amount specified against the applicable Benefit/Optional Benefit in the Certificate of Insurance
and subject always to the availability of the Sum Insured of the respective Benefit or Optional Benefit, as the
case may be.
Claims made under this Policy will be paid on reimbursement basis only or as may be specifically provided for
in the subsequent sections.
Coverage shall be restricted to the Geographical Scope in force for the Insured Person.
The Certificate of Insurance will specify the currency in which claims under the Benefit, Optional Benefits and
Optional Extensions will be made.
Claim documents as specified in Section C.4.3 is applicable to each and every claim. Additional Claim
documents related to specific Benefit
/ Optional Benefit
/ Optional Extension are mentioned against the
respective Benefit/Optional Benefit/Optional Extension.
B.1. MEDICAL COVER
a) The Certificate of Insurance will specify whether Section B.1(a.1) applies to the Insured Person.
Page 2 of 25
Group Activ Travel - UIN
1. IN-PATIENT CARE WITH DAY/ CARE TREATMENT
If an Insured Person is diagnosed with an Illness or suffers an Injury whilst on a Trip during the Period of Insurance
that solely and directly requires the Insured Person’s Hospitalization or the Insured Person to undergo any of
the Day Care Treatments specified in Annexure - I at a Day Care Centre or Hospital , then We shall indemnify the
Medical Expenses incurred on that Hospitalization or Day Care Treatment provided that:
(i)
The Hospitalization is commenced and continued on the written advice of a Medical Practitioner;
(ii)
The treating Medical Practitioner certifies in writing that the treatment taken for that I llness or
Injury is Medically Necessary Treatment;
(iii)
The treatment for the Illness or Injury commences during the Period of Insurance immediately and
not exceeding 15 days following the diagnosis of the Illness or occurrence of the Injury.
For the purpose of this Benefit, ‘treatment’ shall be deemed to include only the following:
(i)
In patient treatment in a local Hospital at the place the Insured Person is staying at the time of
occurrence of an insured event or at the nearest suitable Hospital.
(ii)
Medical aid that is prescribed by a physician as necessary part of the treatment for broken limbs
or injuries by the Insured Person (e.g. plaster casts, bandages and walking aids).
(iii)
Radiotherapy, heat therapy or phototherapy and other such treatment prescribed by a ph ysician.
(iv)
X-Ray, and other diagnostic tests, provided these pertain to the diagnosed Illness/Injury due to
which Hospitalization was deemed medically necessary.
(v)
Cost of transportation, including necessary medical care en-route, by recognized emergency
service providers/surface Ambulance for medical attention at the nearest Hospital or at the nearest
available Physician.
(vi)
Lifesaving unforeseen emergency measures, or measures solely designed to relieve acute pain,
provided to the Insured Person by medical practitioners.
B.44.OPTIONAL BENEFIT 43 - COVERAGE IN CITY OF RESIDENCE FOR MEDICAL COVER
Where this Benefit is specified in the Policy Schedule/Certificate of Insurance to be in force and applicable for
the Insured Person, the scope of cover for Section B.1(a.1) shall be extended to the duration of transit within
the City of Residence while commencing or concluding a Trip, provided that the Geographical Scope is restricted
to India. In such case, the definition of Period of Insurance in Section D of the P olicy shall stand amended to the
limited extent specified in this Benefit.
2. GENERAL CONDITIONS
The following General Conditions shall be applicable to Benefit - ‘Medical Cover’, all Optional Benefits, Optional
Extension and Specific Policy Terms & Conditions under the Policy.
C.2.1. The Insured Person’s cover under the Policy shall not attach to any journey that has already commenced
prior to the Policy Period Start Date or prior to the commencement of the Insured Person’s cover under the
Policy.
C.2.5. This product may be withdrawn / modified by Us after due approval from the IRDA of India. In case this
product is withdrawn / modified by Us, this Policy can be extended under the then prevailing product or its
nearest substitute filed with and approved by IRDA of India. We shall duly intimate You at least three months
prior to the date of such withdrawal / modification of this product and the options available to You at the time
of extension of this policy.
C.2.9. Cancellation / Termination - At Your request, the Certificate of Insurance shall be cancelled any time prior
to the Period of Insurance End Date specified in the Certificate of Insurance subject to the following conditions:
(b) Cancellation of Certificate of Insurance, issued for a Single Trip, at a date earlier than the Period of Insurance
End Date specified in Certificate of Insurance can be done only if the Insured Person returns to the Country of
Residence/City of Residence before the Period of Insurance End Date.
Refund of premium shall only be applicable if the difference between the arrival date to the Country of Residence
and the Certificate of Insurance End Date is at least 1 day. Premium refunded shall be the difference of the
amount of premium paid for the original Period of Insura nce and the premium applicable by taking the arrival
date as the new Period of Insurance End Date.
Page 3 of 25
Group Activ Travel - UIN
(d) No refund of premium shall be eligible in case of cancellation of this Certificate of Insurance where a Claim
has been incurred/ registered. We shall have no liability to make payment of any claims which are incurred post
cancellation of the Certificate of Insurance.
3. PERMANENT EXCLUSIONS
(applicable to Benefit
- ‘Medical Cover’, all Optional Benefits & Optional
Extensions)
Any Claim in respect of any Insured Person for, arising out of or directly or indirectly due to any of the following
shall not be admissible unless expressly stated to the contrary elsewhere in the Policy terms and conditions:
(a) Any condition or treatment as specified in Annexure - II.
(b) Treatment in any Hospital or by any Medical Practitioner or any other provider of services that We have
(c) Any events occurring outside the Period of Insurance
(d) The Insured Person:
(i) traveling against the advice of a Medical Practitioner; or
(ii) receiving medical treatment
(or has planned to receive during the Policy Term for an existing illness/
diagnose/ condition); or
(iii) travelling for the purpose of obtaining medical treatment; or
(iv) taking part or is supposed to participate in a naval, military or air force operation or war like or peace keeping
operation.
(v) traveling to any country for which his/her visa is not allotted.
(e) An act of self-destruction or self-inflicted Injury, attempted suicide or suicide while sane or insane.
(f) Any Illness or Injury directly or indirectly resulting or arising from or occurring during the commission of any
breach of any law by the Insured Person with any criminal intent.
(g) Any condition directly or indirectly caused by or associated with any sexually transmitted disease, including
Genital Warts, Syphilis, Gonorrhoea, Genital Herpes, Chlamydia, Pubic Lice and Trichomoniasis, Acquired
Immuno Deficiency Syndrome (AIDS) whether or not arising out of HIV, Human T-Cell Lymphotropic Virus Type
III (HTLV-III or IITLB-III) or Lymphadinopathy Associated Virus (LAV) or the mutants derivative or Variations
Deficiency Syndrome or any Syndrome or condition of a similar kind .
(h) Any treatment arising from or traceable to pregnancy (including voluntary termination), miscarriage (unless
due to an Accident), childbirth, maternity (including caesarean section), abortion or complications of any of
these. This exclusion shall not apply to ectopic pregnancy, which is proved by diagnostic means and certification
by a gynaecologist that it is life threatening.
(i) Any treatment arising from or traceable to any fertility, infertility, sub fertility or assisted conception
procedure or sterilization or procedure, birth control procedures, hormone replacement therapy, contraceptive
supplies or services including complications arising due to supplying services or Assisted Reproductive
Technology.
(j) Any treatment or surgery for any dental Illness or Injury.
(k) Treatment taken from anyone who is not a Medical Practitioner or from a Medical Practitioner who is
practicing outside the discipline for which he is licensed or any kind of self-medication.
(l) Charges incurred in connection with cost of spectacles and contact lenses, hearing aids, routine eye and ear
examinations, laser surgery for correction of refractory errors, dentures, artificial teeth and all other similar
external appliances and or devices whether for
diagnosis or treatment.
(m) Unproven / Experimental Treatment which are not consistent with or incidental to the diagnosis and
treatment of the positive existence or presence of any Illness for which confinement is required at a Hospital.
Any Illness or treatment which is a result or a consequence of undergoing such experimental or unproven
treatment.
(n) Any expenses incurred on prosthesis, corrective devices, external durable medical equipment of any kind,
like wheelchairs, walker, belts, collar, caps, splints, braces, stockings of any kind, diabetic footwear, glucometer
or thermometer, crutches, ambulatory devices, instruments used in treatment of sleep apnea syndrome
(C.P.A.P) or continuous ambulatory peritoneal dialysis (C.A.P.D.) and oxygen concentrator for asthmatic
condition, cost of cochlear implants.
(o) Weight management services and treatment, vitamins and tonics related to weight control programmers,
services and supplies including treatment of obesity (including morbid obesity).
Page 4 of 25
Group Activ Travel - UIN
(p) Any treatment related to sleep disorder or sleep apnea syndrome, general debility convalescence, cure, rest
cure, health hydros, nature cure clinics, sanatorium treatment, rehabilitation measures, private duty nursing,
respite care, long-term nursing care, custodial care or any treatment in an establishment that is not a Hospital.
(q) Treatment of all external Congenital Anomalies or Illness or defects or anomalies or treatment relating to
external birth defects.
(r) Treatment of mental Illness, stress, psychiatric or psychological disorders.
(s) Aesthetic treatment, cosmetic surgery and plastic surgery or related treatment of any description, including
any complication arising from these treatments, other than as may be necessitated due to an Injury.
(t) Any treatment or surgery for change of sex or gender reassignments including any complication arising from
these treatments.
(u) Circumcision unless necessary for treatment of an Illness or as may be necessitated due to an Accident.
(v) All preventive care, vaccination, including inoculation and immunizations (except in case of post-bite
treatment), vitamins and tonics.
(w) Artificial life maintenance, including life support machine used to sustain a person, who has been declared
brain dead, or is demonstrating any of the following conditions :
1. Deep coma and unresponsiveness to all forms of stimulation; or
2. Absent pupillary light reaction; or
3. Absent oculovestibular and corneal reflexes; or
4. Complete apnea.
(x) All expenses related to donor screening, treatment, including surgery to remove organs from the donor, in
case of transplant surgery.
(y) Non-allopathic treatment.
(z) Illness or Injury attributable to the consumption, use, misuse or abuse of tobacco, intoxicating drugs or
alcohol.
(aa) Charges incurred at a Hospital primarily for diagnostic, X-ray or laboratory examinations not consistent with
or incidental to the diagnosis and treatment of the positive existence or presence of any Illness or Injury, for
which in-patient care or a day care procedure is required.
(bb)War (whether declared or not) and war like occurrence or invasion, acts of foreign enemies, hostilities, civil
war, rebellion, revolutions, insurrections, mutiny, military or usurped power, seizure, capture, arrest, res traints
and detainment of all kinds.
(cc) Stem cell implantation, harvesting, storage or any kind of treatment using stem cells.
(dd)Nuclear, chemical or biological attack or weapons, contributed to, caused by, resulting from or from any
other cause or event contributing concurrently or in any other sequence to the loss, claim or expense. For the
purpose of this exclusion:
(i) Nuclear attack or weapons means the use of any nuclear weapon or device or waste or combustion of nuclear
fuel or the emission, discharge, dispersal, release or escape of fissile or fusion material emitting a level of
radioactivity capable of causing any Illness, incapacitating disablement or death.
(ii) Chemical attack or weapons means the emission, discharge, dispersal, release or escape of any solid, liquid
or gaseous chemical compound which, when suitably distributed, is capable of causing any Illness, incapacitating
disablement or death.
(iii) Biological attack or weapons means the emission, discharge, dispersal, release or escape of any pathogenic
(disease producing) micro-organisms and/or biologically produced toxins (including genetically modified
organisms and chemically synthesized toxins) which are capable of causing any Illness, incapacitating
disablement or death.
In addition to the foregoing, any loss, claim or expense of whatsoever nature directly or indirectly arising out of,
contributed to, caused by, resulting from, or in connection with any action taken in controlling, preventing,
suppressing, minimizing or in any way relating to the above is also excluded.
(ee) Impairment of an Insured Person’s intellectual faculties by abuse of stimulants or depressants͘
(ff) Any sporting activities in so far as they involve the training or participation in competitions of professiona l
or semi-professional sports persons.
(gg) Any Claim relating to Adventure Sports.
(hh) Any Medical Expenses or other expenses which are not Reasonable and Customary Charges.
(ii) Any procedure or diagnostic test for gender detection of foetus/unborn child.
4. CLAIM INTIMATION, ASSESSMENT AND MANAGEMENT
Page 5 of 25
Group Activ Travel - UIN
Upon the occurrence of any event, Illness or Injury that may give rise to a Claim under this Policy, then as a
Condition Precedent to Our liability under the Policy, You or Insured Person (or the Nominee or legal heir if the
Insured Person is deceased) shall undertake all the following in addition to any specific requirements specified
within the Benefit/Optional Benefit/Optional Extension under which the Claim is made:
4.1. Claims Intimation
(a) If any Illness is diagnosed or discovered or any Injury is suffered or any other contingency occurs which has
resulted in a Claim or may result in a Claim under the Policy, You or Insured Person (or the Nominee or legal heir
if the Insured Person is deceased), shall notify Us either at Our call center or in writing immediately and in any
event within the timeframe (if any) specified in the Benefit/Optional Benefit under which the Claim is made.
(b) It is agreed and understood that the following details are to be provided to Us at the time of intimation of
the Claim:
(i) Policy Number and Certificate of Insurance;
(ii) Claimant’s Name;
(iii) Name of the Insured Person in respect of whom the Claim is being made;
(iv) Nature of Illness or Injury or contingency for which Claim is being made and the Benefit and/or Optional
Benefit and/or Optional Extension under which the Claim is being made;
(v) Date of admission to Hospital or loss;
(vi) Name and address of the attending Medical Practitioner and Hospital (if applicable);
(vii) Any other information, documentation or details requested by Us or the Assistance Service Provider.
(c) Any event that may give rise to a Claim under a Hospitalization benefit has to be notified to Us or the
Assistance Service Provider, within 48 hours of Hospitalization or before discharge (whichever is earlier).
However, We shall examine and relax the timeframe specified for Claim intimation depending upon whether
the reasons for delay are beyond the control of the claimant.
4.2. Claims Procedure
(c) Reimbursement:
(i) It is agreed and understood that in all cases where intimation of a Claim has been provided under this
provision, all the information and documentation specified against the Benefit / Optional Benefit and Section C.
4͘3 below shall be submitted (at the Insured Person’s expense) to us immediately and in any event within 30
days of Insured Person’s discharge from Hospital or completion of treatment or date of loss, whichever is later͘
4.3. Claim Documentation
You or Insured Person (or Nominee or legal heir if the Insured Person is deceased) shall (at his /her expense) give
the documentation specified below and any additional information or documentation specified in the Benefit
and/or Optional Benefit and/or Optional Extension under which the Claim is being made to Us or the Assistance
Service Provider immediately and in any event within 30 days of the occurrence of the Injury/Illness or treatment
or loss.
(i) Duly completed and signed Claim form, in original;
(ii) Copy of first and last page of passport copy with entry/exit stamp;
(iii) Any other document as required by Us or Assistance Service Provider;
(iv) Additional documents as specified for each Benefit.
(v) Original pathological or diagnostic reports, discharge summary, Day Care summary, indoor case papers and
prescriptions issued by the treating Medical Practitioner or Hospital as applicable.
(vi) Copy of e-ticket / boarding pass.
(vii) NEFT / banking details along with cancelled cheque copy for Insured Person / Nominee (where applicable)
with pre-printed name; if name is not pre-printed please provide copy of bank passbook / bank statement.
Note: ll invoices and bills should be in Insured Person’s name or as per the documents mentioned in the
respective Benefit/Optional Benefits. Depending on the nature of the Claim, treatment undertaken or illness,
there would be a possibility of seeking more information / document from the Claimant concerned without
prejudice to his interest and the same shall be requested by any means of recognized communication channels.
However, claims filed even beyond the timelines mentioned above will be considered if there are valid reasons
for the delay.
4.4. Policyholder’s or Insured Person’s or Claimant’s duty at the time of Claim
It is agreed and understood that as a Condition Precedent to Our liability in respect of a Claim to be considered
under this Policy:
(a) All reasonable steps and measures must be taken to avoid or minimize the quantum of any Claim that may
be made under this Policy.
Page 6 of 25
Group Activ Travel - UIN
(b) The Insured Person shall follow the directions, advice or guidance provided by a Medical Practitioner and We
shall not be obliged to make payment that is brought about or contributed to by the Insured Person failing to
follow such directions, advice or guidance.
(c) Intimation of the Claim, notification of the Claim and submission or provision of all information and
documentation shall be made promptly and in any event in accordance with the procedures and within the
timeframes specified in Section C.4 of the Policy and the specific procedures and timeframes specified under the
respective Benefit or Optional Benefit or Optional Extension under which the Claim is being made.
(d) The Insured Person shall, at Our request and at Our cost and expense, submit himself / herself for a medical
examination by Our/ ssistance Service Provider’s nominated Medical Practitioner as often as We consider
reasonable and necessary.
(e) We/ ssistance Service Provider’s Medical Practitioner and representatives shall be given access and co -
operation to inspect the Insured Person’s medical and Hospitalization records and to investigate the facts and
examine the Insured Person.
(f) We shall be provided with complete documentation and information which We have requested to establish
Our liability for the Claim, its circumstances and its quantum.
(g) Report any information/document which helps the insurance system to eliminate bad practices in the market.
4.5. Claim Assessment
(a) All admissible Claims under this Policy shall be assessed by Us in the following progressive order:
i. If the provisions of the Contribution Section in Section C.13 are applicable, Our liability to make payment under
that Claim shall first be apportioned accordingly.
ii. If any sub-limits on Medical Expenses are applicable in accordance with Section B.1 (b) (xi), Our liability to
make payment shall be limited to such extent as appli cable.
iii. The Deductible shall be applied to each Claim that is either paid or payable (and not excluded), under this
Policy. Our liability to make payment shall commence only once the amount of the Claim payable or paid exceeds
the Deductible.
iv. Co-payment shall be applicable on the amount payable by Us after applying Section C.4.5(a) (i), (ii) and (iii).
4.6. Payment terms
(a) We may change the Assistance Service Provider or utilize the service of any other assistance service provider
by giving written notification to You.
(b)The obligation of the Company to make payments to the Insured Person in respect of claims made shall be
to make payment in Indian Rupees and after the Insured Person’s return to India only. For all admissible
Claims, the exchange rate as follows shall be applied:
(i)
Reimbursement (indemnity) - Date of Invoice
(ii)
Fixed Benefit - Date of occurrence of insured event.
(c) If the Assistance Service Provider or We request that bills or vouchers in a local language or vernacular be
accompanied by an appropriate translation into English then the costs of such translation must be borne by You
or the Insured Person.
(d) The Sum Insured of the Insured Person shall be reduced by the amount payable or paid under the Policy
Terms and Conditions or any Benefit / Optional Benefit / Optional Extension applicable under this Policy and
only the balance amount shall be available as the Sum Insured for the unexpired Period of Insurance for the
Insured Person.
(e) We shall have no liability to make payment of a Claim under the Policy in respect of an Insured Person, once
the Sum Insured for that Insured Person is exhausted or if the benefi t amount under the applicable
Benefit/Optional Benefit/Optional Extension as specified in the Policy Schedule/Certificate of Insurance is
exhausted.
(f) If the Insured Person suffers a relapse within 45 days of the date of discharge from the Hospital for which a
Claim has been made, then such relapse shall be deemed to be part of the same Claim and all the limits for Any
One Illness under this Policy shall be applied as if they were under a single Claim.
(g) For Cashless Facility Claims, the payment shall be made to the Network Provider whose discharge would be
complete and final.
(h) For the reimbursement Claims, We shall pay to the Insured Person unless specified otherwise in the
Certificate of Insurance. In the event of death of the Insured Person, unles s specified otherwise in the Certificate
of Insurance, We shall pay to the Nominee (as named in the Certificate of Insurance) and in case of no Nominee
to the legal heir of the Insured Person whose discharge shall be treated as full and final discharge of its liability
under the Policy.
Page 7 of 25
Group Activ Travel - UIN
(i) All claims will be investigated (as required) and settled or rejected in accordance with the applicable
regulatory guidelines, including the IRDAI (Protection of Policyholders Interests) Regulations, 2017. We shall
settle or reject any Claim under the Policy within 30 days of receipt of the last necessary document/ information
as required for settlement of such Claim and sought by Us. In case there is delay in the payment of any claim
that has been admitted as payable by Us under the Policy, beyond the time period as prescribed under IRDAI
(Protection of Policyholders Interests) Regulations, 2017, We shall pay additional amount as interest at a rate
which is 2% above the bank rate prevalent at the beginning of the financial year in which the claim has fallen
due͘ For the purpose of this clause, ‘bank rate’ shall mean the existing bank rate as notified by Reserve Bank of
India, unless the extant regulation requires payment based on some other prescribed interest rate.
(j) No loading based on individual claim experience shall be applicable on Renewal premium payable in case of
Annual Trip cover.
5. Disclosure to Information Norm
If any untrue or incorrect statements are made or there has been a misrepresentation, mis -description or non-
disclosure of any material particulars or any material information having been withheld, or if a Claim is
fraudulently made or any fraudulent means or devices are used by You, the Insured Person or any one acting on
his or their behalf, We shall have no liability to make payment of any Claims and the premium paid shall be
forfeited to Us on cancellation of the Policy.
6. Observance of Terms and Conditions
The due observance and fulfilment of the terms and conditions of this Policy (including the realization of
premium by their respective due dates and compliance with the specified procedure on all Claims) in so far as
they relate to anything to be done or complied with by You or any Insured Person, shall be Condition Precedent
to Our liability under the Policy.
7. Reasonable Care
Insured Persons shall take all reasonable steps to safeguard the interests against any Illness or Injury or any
other loss that may give rise to a Claim.
8. Material Change
It is a Condition Precedent to Our liability under the Policy that You shall immediately and in any case within 7
days notify Us in writing of any material change in the risk on account of change in occupation or business of the
Insured Person at its own expense, as per Annexure -III. We may adjust the scope of cover and / or the premium
paid or payable, accordingly.
9. Records to be maintained
You and Insured Person shall keep an accurate record containing all relevant medical records and shall allow Us
or Our representatives to inspect such records. You or Insured Person shall furnish such information as We may
require under this Policy at any time during the Policy Period or until final adjustment (if any) and resolution of
all Claims under this Policy.
10. No constructive Notice
Any knowledge or information of any circumstance or condition in relation to You or Insured Person which is in
possession of Us other than that information expressly disclosed in the Proposal Form or otherwise in writing to
Us, shall not be held to be binding or prejudicially affect Us.
11. Complete Discharge
Payment made by Us to the Insured Person or the Nominee or the legal heir or representative of the Insured
Person, as the case may be, under the Policy shall in all cases be complete and construe as an effectual discharge
in favor of Us.
12. Subrogation
You and Insured Person shall at his/her own expense do or concur in doing or permit to be done all such acts
and things that may be necessary or reasonably required by Us for the purpose of enforcing and / or securing
any civil or criminal rights and remedies or obtaining relief or indemnity from any other party to which We are
or would become entitled upon Us paying for a Claim under this Policy, whether such acts or things shall be or
become necessary or required before or after its payment. Neither You nor any Insured Person shall prejudice
these subrogation rights in any manner and shall at his /er own expense provide Us with whatever assistance or
cooperation is required to enforce such rights. This clause shall not apply to any Benefit or Optional Benefit or
Optional Extension offered on a fixed benefit basis.
13. Contribution
(a) In case any Insured Person is covered under more than one indemnity insurance policies, with Us or with
other insurers, You/Insured Person shall have the right to settle the Claim with any of Us, provided that the
Claim amount payable is up to the sum insured of such Policy.
Page 8 of 25
Group Activ Travel - UIN
(b) In case the Claim amount under a single policy exceeds the Sum Insured after considering the deductible or
co-payment, then the Insured Person shall have the right to choose the companies with whom the Claim is to
be settled.
This clause shall not apply to any Benefit or Optional Benefit or Optional Extension offered on a fixed benefit
basis.
14. Policy Disputes
Any and all disputes or differences under or in relation to the validity, construction, interpretation and effect to
this Policy shall be determined by the Indian Courts and in accordance with Indian law.
15. Cancellation / Termination
We may at any time, cancel this Policy on grounds as specified in Section C.5 and We shall have no liability to
make payment of any claims and the premium paid shall be forfeited, by giving 15 days’ notice in writing by
Registered Post Acknowledgment Due / recorded delivery to You at Your last known address.
16. Communication
(a) Any communication meant for Us must be in writing and be delivered to Our address shown in the Policy
Schedule/Certificate of Insurance. Any communication meant for You or the Insured Person shall be sent by Us
to Your last known address or the address as shown in the Policy Schedule/Certificate of Insurance (as
applicable).
(b) All notifications and declarations for Us must be in writing and sent to the address specified in the Policy
Schedule/ Certificate of Insurance. Agents are not authorized to receive notices and declarations on Our behalf.
(c) Notice and instructions shall be deemed served 10 days after posting or immediately upon receipt in the case
of hand delivery, facsimile or e-mail.
17. Alterations in the Policy
This Policy constitutes the complete contract of insurance. No change or alteration shall be valid or effective
unless approved in writing by Us, which approval shall be evidenced by a written endorsement signed and
stamped by Us.
18. Cause of Action
No Claims shall be payable under this Policy unless the event or occurrence giving rise to the Claim occurs in the
Geographical Scope specified in the Certificate of Insurance.
19. Overriding effect of Policy Schedule / Certificate of Insurance
In case of any inconsistency in the terms and conditions in this Policy vis-a-vis the information contained in the
Policy Schedule and/or Certificate of Insurance, the information contained in the Policy Schedule or Certificate
of Insurance shall prevail.
20. Electronic Transactions
You and Insured Person agrees to adhere to and comply with all such terms and conditions as We may prescribe
from time to time, and hereby agrees and confirms that all transactions effected by or through facilities for
conducting remote transactions including the Internet, World Wide Web, electronic data interchange, call
centers, tele-service operations (whether voice, video, data or combination thereof) or by means of electronic,
computer, automated machines network or through other means of telecommunication, established by or on
behalf of Us, for and in respect of the Policy or its terms, or Our other products and services, shall constitute
legally binding and valid transactions when done in adherence to and in compliance with the Our terms and
conditions for such facilities, as may be prescribed from time to time.
21. Grievances
In case of a grievance, the Insured Person/ You can contact Us with the details through:
Our website: adityabirlahealth.com/healthinsurance
Email: customercare.abh@adityabirlacapital.com
Toll Free: 1800 270 7000
Address: Aditya Birla Health Insurance Co. Limited
10th Floor, Rtech, Nirlon IT park, Western Express highway,
Goregaon East, Mumbai - 400063
For senior citizens, please contact Our respective branch office or call at 1800 103 1033 or write an e - mail at
The Insured Person/You can also walk-in and approach the grievance cell at any of Our branches. If in case the
Insured Person/You is not satisfied with the response then they can contact Our Head of Customer Service at
Page 9 of 25
Group Activ Travel - UIN
If the Insured Person/You is not satisfied with Our redressal, he/she may use the Integrated Grievance
Management Services (IGMS). For registration in IGMS please visit IRDAI website www.irda.gov.in
If the Insured Person/You are still not satisfied, he/she may approach the nearest Insurance Ombudsman. The
contact details of the Ombudsman offices are provided on Our website and in this Policy at Annexure A
Section D. DEFINITIONS
The terms and conditions, benefits, exclusions, various procedures and conditions which have been built in to
the Policy are to be construed in accordance with the applicable provisions contained in the Policy. The terms
defined below have the meanings ascribed to them wherever they appear in this Policy and, where appropriate,
references to the singular include references to the plural; references to the male include the female and
references to any statutory enactment include subsequent cha nges to the same and vice versa.
1. Accident is a sudden, unforeseen and involuntary event caused by external, visible and violent means;
2. Adventure Sports shall mean any sport or activity, which is potentially dangerous to the Insured Person
whether he is trained or not. Such sport/activity includes racing and competitions, stunt activities of any kind,
adventure racing, base jumping, blathlon, big game hunting, black water rafting, BMX stunt/ obstacle riding,
bobsleighing/ using skeletons, bouldering, boxing, canyoning, caving/ pot holing, cave tubing, rock climbing/
trekking/ mountaineering, cycle racing, cyclo cross, drag racing, endurance testing, hand gliding, harness racing,
hell skiing, high diving (above 5 meters), hunting, ice hockey, ice speedway, jousting, judo, karate, kendo,
lugging, risky manual labor, marathon running, martial arts, micro - lighting, modern pentathlon, motor cycle
racing, motor rallying, parachuting, paragliding/ parapenting, piloting aircraft, polo, power lifting, power boat
racing, quad biking, river boarding, scuba diving, river bugging, rodeo, roller hockey, rugby, ski acrobatics, ski
doo ski jumping, ski racing, sky diving, small bore target shooting, speed trials/ time trials, triathlon, water ski
jumping, weight lifting, wrestling and activities of similar nature;
3. Age means the completed age of the Insured Person on his last birthday;
4. Ambulance means a road vehicle or aircraft operated by a licensed / authorized service provider only and
equipped for the transport and paramedical treatment of the person requiring medical attention;
5. Annual Multi Trip Cover means a cover under the Policy under which there can be more than one Period of
Insurance for the Insured Person during the Policy Period, subject to the maximum trip duration (per trip)
specified on the Policy Schedule/ Certificate of Insurance or as opted;
6. Any one Illness means a continuous period of illness and it includes relapse within 45 days from the date of
last consultation with the Hospital / Nursing Home where the treatment may have been taken;
7. Assistance Service Provider means the service provider specified in the Policy Schedule and/or Certificate of
Insurance, appointed by Us from time to time;
8. Cashless facility means a facility extended by the insurer to the insured where the payments, of the costs of
treatment undergone by the insured in accordance with the policy terms and conditions, are directly made to
the network provider by the insurer to the extent pre-authorization approved;
9. Certificate of Insurance means the certificate We issue to an Insured Person evidencing cover under the
Policy;
10. Checked-In Baggage means the baggage (luggage and personal possessions belonging to or in the lawful
custody of the Insured Person) offered by the Insured Person and accepted for custody by a Common Carrier for
transportation in the same Common Carrier in which the Insured Person is travelling and for which the Common
Carrier has provided a baggage receipt, and the contents of the baggage checked-in by the Insured Person as
long as such contents do not violate any policy or rule restricting the nature of items that may be carried on
board. This shall exclude all the items that are carried/ transported under a contract of affreightment;
11. City of Residence means and includes any city, town or village in which the Insured Person is currently
residing in India and as specified in the Insured Person’s corresponding address in the Policy Schedule/Certificate
of Insurance;
12. Claim means a demand made in accordance with the terms and conditions of the Policy for payment under
a Benefit or Optional Benefit or Optional Extension in respect of an Insured Person;
13. Company (also referred as We/Us/Our) means the Aditya Birla Health Insurance Company Limited;
14. Common Carrier means any civilian land or water conveyance or scheduled aircraft operated under a valid
license for the transportation of fare paying passengers under a valid ticket;
15. Condition Precedent means a policy term or condition upon which the Insurer’s liability under the policy is
conditional upon;
Page 10 of 25
Group Activ Travel - UIN
16. Congenital Anomaly refers to a condition(s) which is present since birth, and which is abnormal with
reference to form, structure or position.
a) Internal Congenital Anomaly
Congenital anomaly which is not in the visible and accessible parts of the body
b) External Congenital Anomaly
Congenital anomaly which is in the visible and accessible parts of the body;
17. Co-payment is a cost-sharing requirement under a health insurance policy that provides that the
policyholder/insured shall bear a specified percentage of the admissible claim amount. A co-payment does not
reduce the sum insured;
18. Country of Residence means the country in which the Insured Person is currently residing and as specified
in the Insured Person’s corresponding address as specified in the Policy Schedule or Certificate of Insurance,
which for the purpose of thi s Policy shall be India;
19. Damages means sums payable following judgments or awards but shall not include fines, penalties, punitive
damages, exemplary damages, any non-pecuniary relief, or any other amount for which an Insured Person is not
financially liable, or which is without legal recourse to the Insured Person, or any matter that may be deemed
to be uninsurable under Indian Law;
20. Day Care Centre means any institution established for day care treatment of illness and/or injuries or a
medical setup within a Hospital and which has been registered with the local authorities, wherever applicable,
and is under the supervision of a registered and qualified Medical Practitioner AND must comply with all
minimum criteria as under—
a) has qualified nursing staff under its employment;
b) has qualified Medical Practitioner/s in charge;
c) has a fully equipped operation theatre of its own where surgical procedures are carried out;
d) maintains daily records of patients and shall make these accessible to the insurance company’s authorized
personnel;
21. Day Care Treatment refers to medical treatment, and/or surgical procedure as specified under Annexure I
which is:
a) undertaken under General or Local Anesthesia in a hospital/day care center in less than 24 hour s because of
technological advancement, and
b) which would have otherwise required a hospitalization of more than 24 hours.
Treatment normally taken on an out-patient basis is not included in the scope of this definition;
22. Deductible means a cost-sharing requirement under a health insurance policy that provides that the insurer
will not be liable for a specified rupee / applicable currency amount in case of indemnity policies and for a
specified number of days/hours in case of hospital cash policies which will apply before any Benefits are payable
by the insurer. A deductible does not reduce the Sum Insured;
23. Dental Treatment means a treatment related to teeth or structures supporting teeth including examinations,
fillings (where appropriate), crowns, extractions and surgery;
24. Dependent Child means a child (natural or legally adopted), who is:
a) Financially dependent on the Insured Person;
b) Does not have his independent sources of income; and
c) Has not attained Age 25 years;
25 Disclosure to information norm: The policy shall be void and all premium paid hereon shall be forfeited to
the Company, in the event of misrepresentation, mis -description or non-disclosure of any material fact;
26. Emergency Care means management for an illness or injury which results in symptoms which occur suddenly
and unexpectedly, and requires immediate care by a medical practitioner to prevent death or serious long term
impairment of the insured person’s health;
27. Family means and includes the Insured Person’s legal spouse and upto 2 dependent children upto age 25
years ;
28. Geographical Scope means the countries or geographical boundaries in which the coverage under the Policy
is valid as specified in the Policy Schedule/ Certificate of Insurance;
29. Grace Period means the specified period of time immediately following the premium due date during which
payment can be made to renew or continue a policy in force without loss of continuity benefits such as waiting
periods and coverage of pre-existing diseases. Coverage is not available for the period for which no premium is
received;
30. Hijack means any act of unlawful seizure or control of a Common Carrier with a wrongful intent using force
or violence or threat thereof;
Page 11 of 25
Group Activ Travel - UIN
31. Burglary means any act of actual, forcible and violent entry and or exit from the premises of the Insured
Person with intent to commit an act of crime or theft.
32. Hospital means any institution established for in-patient care and day care treatment of illness and/or
injuries and which has been registered as a hospital with the local authorities under the Clinical Establishments
(Registration and Regulation) Act, 2010 or under the enactments specified under the Schedule of Section 56(1)
of the said Act OR complies with all minimum criteria as under:
a) has qualified nursing staff under its employment round the clock;
b) has at least 10 in-patient beds in towns having a population of less than 10,00,000 and at least 15 inpatient
beds in all other places;
c) has qualified medical practitioner(s) in charge round the clock;
d) has a fully equipped operation theatre of its own where surgical procedures are carried out;
e) maintains daily records of patients and makes these accessible to the insurance company’s authorized
personnel.
or
Any institution established for in- patient care and day care and treatment of Injury or Illness and which has
been registered as a Hospital or a clinic as per law rules and/or regulations applicable for the country where the
contingency arises;
33. Hospitalization means admission in a Hospital for a minimum period of 24 In patient Care consecutive hours
except for specified procedures/ treatments, where such admission could be for a period of less than 24
consecutive hours;
34. Illness means a sickness or a disease or pathological condition leading to the impairment of normal
physiological function which manifests itself during the Policy Period and requires medical treatment.
a. Acute condition - Acute condition is a disease, illness or injury that is likely to respond quickly to treatment
which aims to return the person to his or her state of health immediately before suffering the disease/
illness/ injury which leads to full recovery.
b. Chronic condition - A chronic condition is defined as a dis ease, illness, or injury that has one or more of the
following characteristics:
i. it needs ongoing or long-term monitoring through consultations, examinations, check-ups, and /or
tests
ii. it needs ongoing or long-term control or relief of symptoms
iii.
it requires rehabilitation for the patient or for the patient to be specially trained to cope with it
iv. it continues indefinitely
v. it recurs or is likely to recur
35. Immediate Family Member means an Insured Person’s lawful spouse, Dependent Children and parents only;
36. Injury means accidental physical bodily harm excluding Illness or disease solely and directly caused by
external, violent and visible and evident means which is verified and certified by a Medical Practitioner;
37. Inpatient Care means treatment for which the insured person has to stay in a hospital for more than 24
hours for a covered event;
38. Intensive Care Unit means an identified section, ward or wing of a Hospital which is under the constant
supervision of a dedicated Medical Practitioner(s), and which is specially equipped for the continuous monitoring
and treatment of patients who are in a critical condition, or require life support facilities and where the level of
care and supervision is considerably more sophisticated and intensive than in the ordinary and other wards;
39. ICU Charges means the amount charged by a Hospital towards ICU expenses which shall include the expenses
for ICU bed, general medical support services provided to any ICU patient including monitoring devices, critical
care nursing and intensivist charges.
40. Insured Person means a person whose name specifically appears under Insured in the Certificate of
Insurance and is a covered group member;
41. Life Threatening Medical Condition means a medical condition suffered by the Insured Person which has
the following characteristics:
a) Markedly unstable vital parameters (blood pressure, pulse, temperature and respiratory rate); or
b) Acute impairment of one or more vital organ systems (involving brain, heart, lungs, liver, kidneys and
pancreas); or
c) Critical care being provided, which involves high complexity decision making to assess, manipulate and
support vital system functions to treat single or multiple vital organ failures and requires interpretation of
multiple physiological parameters and application of advanced technology; or
d) Critical care being provided in critical care area such as coronary care unit, Intensive Care Unit, respiratory
care unit, or the emergency department;
Page 12 of 25
Group Activ Travel - UIN
and certified in writing by the attending Medical Practitioner as a Life Threatening Medical Condition;
42. Man Day means every completed 24 hrs per Insured Person from the start date of Period of Insurance which
falls within the Period of Insurance.
43. Maternity expenses shall include—
a) medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean sections
incurred during hospitalization).
b) expenses towards lawful medical termination of pregnancy during the policy period;
44. Medical Advice means any consultation or advice from a Medical Practitioner including the issuance of any
prescription or follow-up prescription;
45. Medical Evacuation means the removal of the Insured Person from the site of Accident or Illness to a nearest
Hospital where necessary medical care can be accorded to him/her, including medical care required en route.
46. Medical Expenses means those expenses that an Insured Person has necessarily and actually incurred for
medical treatment on account of Illness or Accident on the advice of a Medical Practitioner, as long as these are
no more than would have been payable if the Insured Person had not been insured and no more than other
Hospitals or doctors in the same locality would have charged for the same medical treatment;
47. Medical Practitioner means a person who holds a valid registration from the medical council of any State
and is thereby entitled to practice medicine within its jurisdiction; and is acting within the scope and jurisdiction
of license. The term Medical Practitioner includes a physician and / or surgeon;
48. Medically Necessary Treatment means any treatment, tests, medication, or stay in Hospital or part of a stay
in Hospital which:
i. Is required for the medical management of the Illness or Injury suffered by the Insured Person;
ii. Must not exceed the level of care necessary to provide safe, adequate and appropriate medical care in scope,
duration, or intensity;
iii. Must have been prescribed by a Medical Practitioner;
iv. Must conform to the professional standards widely accepted in international medical practice or by the
medical community in India.
49. Network Provider means Hospitals or Health Care providers enlisted by an insurer or by an Assistance Service
Provider and insured together to provide services to an insured on payment by a cashless facility;
50. Nominee means the person named in the Certificate of Insurance to receive the benefits payable under this
Policy if the Insured Person is deceased. For the purpose of avoidance of doubt it is cl arified that if the Nominee
is a minor on the date when payment becomes due under the Policy, payment shall be made to the Appointee
named in the Certificate of Insurance;
51. Non-Network Provider means any hospital, day care centre or other provider that is not part of the network;
52. Notification of Claim means the process of notifying a claim to the insurer or TPA through any of the
recognized modes of communication;
53. OPD Treatment means the one in which the Insured visits a clinic / hospital or associated facility like a
consultation room for diagnosis and treatment based on the advice of a Medical Practitioner. The Insured is not
admitted as a day care or in-patient;
54. Period of Insurance means a period within the Policy Period which commences when the Insured Person
crosses the international border of the Country of Residence if the Geographical Scope is out of India to leave
that country on a Common Carrier or City of Residence if the Geographical Scope is restricted to India to leave
that city and expires automatically on the earliest of:
a) the Insured Person crossing the Indian international border to return to the Country of Residence on a
Common Carrier if the Geographical Scope is out of India or returning to the City of Residence if the Geographical
Scope is restricted to India; or
b) the expiry of the period specified in the Policy Schedule or Certificate of Insurance from the commencement
of the Period of Insurance; or
c) the Policy Period End Date.
55. Place of Destination means the destination place where the journey of the Insured Person, forming part of
the Trip, is scheduled to be concluded through a scheduled Common Carrier;
56. Place of Origin means the starting point/ place from where the Insured Person’s Trip is scheduled to be
undertaken through a Common Carrier by which he finally leaves the Country of Residence or City of Residence;
57. Place of Residence means the dwelling place that the Insured Person is presently resident in as specified as
the correspondence address of the Insured Person in the Policy Schedule or Certificate of Insurance;
58. Policy means these Policy Terms & Conditions, Benefit, Optional Benefits, Optional Extensions (if any), the
Proposal Form, Policy Schedule, Certificate of Insurance, and Annexures which form part of the policy contract
and shall be read together;
Page 13 of 25
Group Activ Travel - UIN
59. Policy Schedule means the certificate attached to and forming part of this Policy;
60. Policyholder (also referred as You) means the person who is the Group Administrator and named in the
Policy Schedule as the Policyholder;
61. Policy Period means the period commencing from the Policy Period Start Date and ending on the Policy
Period End Date as specifically appearing in the Policy Schedule;
62. Policy Period End Date means the date on which the Policy expires, as specified in the Policy Schedule;
63. Policy Period Start Date means the date on which the Policy commences, as specified in the Policy Schedule;
64. Post-natal period is the period beginning immediately after the birth of a child and extending for about six
weeks
65. Pre-existing Disease means any condition, ailment or injury or related condition(s) for which the Insured
Person had signs or symptoms, and/or were diagnosed, and/or received medical advice or treatment within 48
months to prior to the first policy issued by the Company;
66. Pre-Natal period (also known as antenatal care) refers to the regular medical and nursing care recommended
for women during pregnancy
67. Professional Sports means any sporting activity which is undertaken by the Insured Person from which
he/she derives earnings, wage, reward, or profit of any kind.
68. Qualified Nurse is a person who holds a valid registration from the Nursing Council in the respective
jurisdiction;
69. Reasonable and Customary Charges means the charges for services or supplies, which are the standard
charges for the specific provider and consistent with the prevailing charges in the geographical area for identical
or similar services, taking into account the nature of the Illness / Injury involved;
70. Renewal means the terms on which the contract of insurance can be renewed on mutual consent with a
provision of grace period for treating the renewal continuous for the purpose of gaining credit for pre-existing
diseases, time-bound exclusions and for all waiting periods;
71. Robbery means an act of taking or attempting to take anything of value by force, threat of force, or by putting
an individual in fear.
72. Room Rent means the amount charged by a Hospital towards Room and Boarding expenses and shall include
associated Medical Expenses;
73. Single Trip Cover means a cover of the Insured Person under the Policy under which there cannot be more
than one Period of Insurance during the Policy Period;
74. Subrogation shall mean the right of the insurer to assume the rights of the insured person to recover
expenses paid out under the policy that may be recovered from any other source;
75. Sum Insured means:
(a) If the Certificate of Insurance is on individual cover basis, the amount specified in the Certificate of Insurance
which represents Our maximum, total and cumulative liability for any and all Claims under any and all
Benefit/Optional Benefits/Optional Extensions in respect of the Insured Person for the Policy Period.
(b) If the Certificate of Insurance is on family floater basis, the amount specified in the Certificate of Insurance
which represents Our maximum, total and cumulative liability for any and all Claims under any and all
Benefit/Optional Benefits/Optional Extensions in respect of any and all Insured Persons named in the Certificate
of Insurance for the Policy Period.
76. Surgery / Surgical Procedure means manual and / or operative procedure(s) required for treatment of an
Illness or Injury, correction of deformities and defects, diagnosis and cure of diseases, relief of suffering or
prolongation of life, performed in a hospital or a day care centre by a medical practitioner;
77. Terrorism/Terrorist Incident means any actual or threatened use of force or violence directed at or causing
damage, injury, harm or disruption, or commission of an act dangerous to human life or property, against any
individual, property or government, with the stated or unstated objective of pursuing economic, ethnic,
nationalistic, political, racial or religious interests, whether such interests are declared or not. Terrorism shall
also include any act, which is verified or recognized by the relevant Government as an act of terrorism;
78. Trip means planned journey, which starts and ends in the Country of Residence / City of Residence as
mentioned in the Policy Schedule / Certificate of Insurance during the Policy Period except where it is for
emigration purpose
79. Unproven / Experimental Treatment means treatment including drug experimental therapy which is not
based on established medical practice in India, is treatment experimental or unproven.
80. You/Your/Policyholder means the person named in the Policy Schedule as the policyholder and who has
concluded this Policy with Us.
Page 14 of 25
Group Activ Travel - UIN
Page 15 of 25
Group Activ Travel - UIN
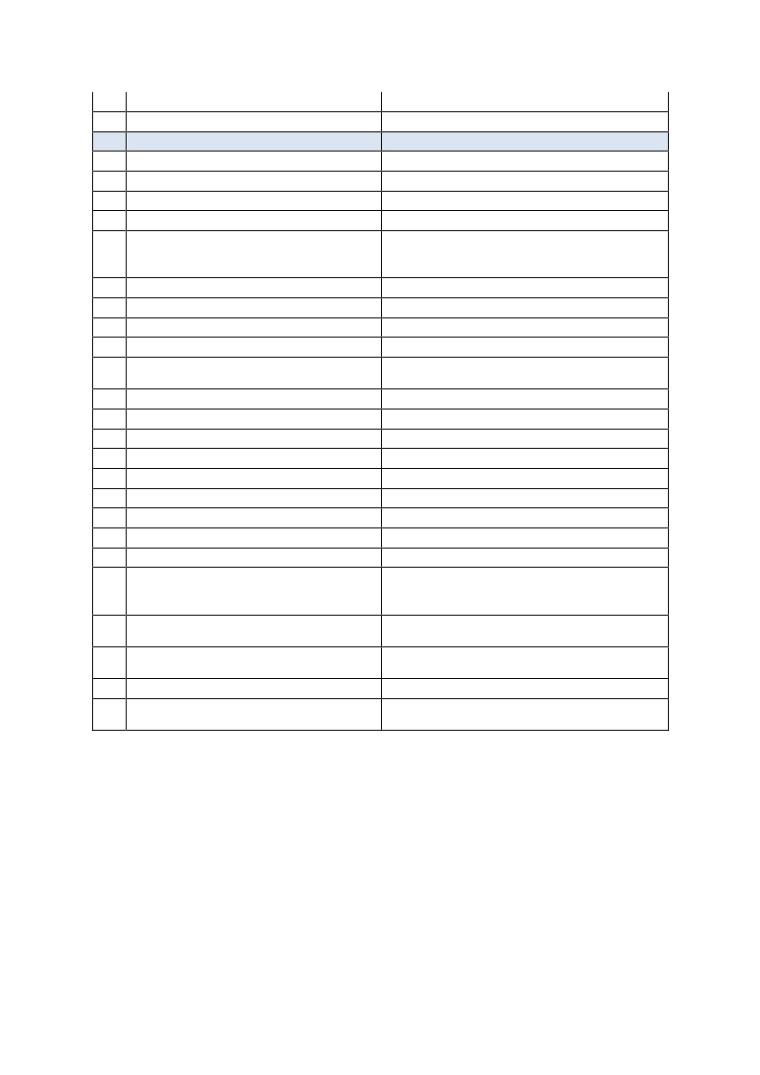
Annexure A: Ombudsmen
CONTACT DETAILS
JURISDICTION OF OFFICE
AHMEDABAD -
Gujarat,
Office of the Insurance Ombudsman,
Dadra & Nagar Haveli,
Jeevan Prakash Building, 6th floor,
Daman and Diu.
Tilak Marg, Relief Road,
Ahmedabad - 380 001.
Tel.: 079 -25501201/02/05/06
BENGALURU
Karnataka.
Office of the Insurance Ombudsman,
Jeevan Soudha Building, PID No. 57-27-N-19
Ground Floor, 19/19, 24th Main Road,
JP Nagar, Ist Phase,
Bengaluru - 560 078.
Tel.: 080 - 26652048 / 26652049
BHOPAL
Madhya Pradesh
Office of the Insurance Ombudsman,
Chattisgarh.
Janak Vihar Complex, 2nd Floor,
6, Malviya Nagar, Opp. Airtel Office,
Near New Market,
Bhopal - 462 003.
Tel.: 0755 - 2769201 / 2769202
Fax: 0755 - 2769203
BHUBANESHWAR
Orissa.
Office of the Insurance Ombudsman,
62, Forest park,
Bhubneshwar - 751 009.
Tel.: 0674 - 2596461 /2596455
Fax: 0674 - 2596429
CHANDIGARH -
Punjab,
Office of the Insurance Ombudsman,
Haryana,
S.C.O. No. 101, 102 & 103, 2nd Floor,
Himachal Pradesh,
Batra Building, Sector 17 - D,
Jammu & Kashmir,
Chandigarh - 160 017.
Chandigarh.
Tel.: 0172 - 2706196 / 2706468
Fax: 0172 - 2708274
CHENNAI -
Tamil Nadu,
Office of the Insurance Ombudsman,
Pondicherry Town and
Fatima Akhtar Court, 4th Floor, 453,
Karaikal (which are part of Pondicherry).
Anna Salai, Teynampet,
CHENNAI - 600 018.
Tel.: 044 - 24333668 / 24335284
Fax: 044 - 24333664
Page 16 of 25
Group Activ Travel - UIN
DELHI -
Delhi.
Office of the Insurance Ombudsman,
2/2 A, Universal Insurance Building,
Asaf Ali Road,
New Delhi - 110 002.
Tel.: 011 - 23239633 / 23237532
Fax: 011 - 23230858
GUWAHATI -
Assam,
Office of the Insurance Ombudsman,
Meghalaya,
Jeevan Nivesh, 5th Floor,
Manipur,
Nr. Panbazar over bridge, S.S. Road,
Mizoram,
Guwahati - 781001(ASSAM).
Arunachal Pradesh,
Tel.: 0361 - 2132204 / 2132205
Nagaland and Tripura.
Fax: 0361 - 2732937
HYDERABAD -
Andhra Pradesh,
Office of the Insurance Ombudsman,
Telangana,
6-2-46, 1st floor, "Moin Court",
Yanam and
Lane Opp. Saleem Function Palace,
part of Territory of Pondicherry.
A. C. Guards, Lakdi -Ka-Pool,
Hyderabad - 500 004.
Tel.: 040 - 65504123 / 23312122
Fax: 040 - 23376599
JAIPUR -
Rajasthan.
Office of the Insurance Ombudsman,
Jeevan Nidhi - II Bldg., Gr. Floor,
Bhawani Singh Marg,
Jaipur - 302 005.
Tel.: 0141 - 2740363
ERNAKULAM -
Kerala,
Office of the Insurance Ombudsman,
Lakshadweep,
2nd Floor, Pulinat Bldg.,
Mahe-a part of Pondicherry.
Opp. Cochin Shipyard, M. G. Road,
Ernakulam - 682 015.
Tel.: 0484 - 2358759 / 2359338
Fax: 0484 - 2359336
KOLKATA -
West Bengal,
Office of the Insurance Ombudsman,
Sikkim,
Hindustan Bldg. Annexe, 4th Floor,
Andaman & Nicobar Islands.
4, C.R. Avenue,
KOLKATA - 700 072.
Tel.: 033 - 22124339 / 22124340
Fax : 033 - 22124341
LUCKNOW -
Districts of Uttar Pradesh :
Office of the Insurance Ombudsman,
Laitpur, Jhansi, Mahoba, Hamirpur, Banda,
6th Floor, Jeevan Bhawan, Phase-II,
Chitrakoot, Allahabad, Mirzapur, Sonbhabdra,
Nawal Kishore Road, Hazratganj,
Fatehpur, Pratapgarh, Jaunpur,Varanasi,
Page 17 of 25
Group Activ Travel - UIN
Lucknow - 226 001.
Gazipur, Jalaun, Kanpur, Lucknow, Unnao,
Tel.: 0522 - 2231330 / 2231331
Sitapur, Lakhimpur, Bahraich, Barabanki,
Fax: 0522 - 2231310
Raebareli, Sravasti, Gonda, Faizabad, Amethi,
Kaushambi, Balrampur, Basti, Ambedkarnagar,
Sultanpur, Maharajgang, Santkabirnagar,
Azamgarh, Kushinagar, Gorkhpur, Deoria, Mau,
Ghazipur, Chandauli, Ballia, Sidharathnagar.
MUMBAI
Goa,
Office of the Insurance Ombudsman,
Mumbai Metropolitan Region
3rd Floor, Jeevan Seva Annexe,
excluding Navi Mumbai & Thane.
S. V. Road, Santacruz (W),
Mumbai - 400 054.
Tel.: 022 - 26106552 / 26106960
Fax: 022 - 26106052
NOIDA -
State of Uttaranchal and the following Districts
Office of the Insurance Ombudsman,
of Uttar Pradesh:
Bhagwan Sahai Palace
Agra, Aligarh, Bagpat, Bareilly, Bijnor, Budaun,
4th Floor, Main Road,
Bulandshehar, Etah, Kanooj, Mainpuri,
Naya Bans, Sector 15,
Mathura, Meerut, Moradabad, Muzaffarnagar,
Distt: Gautam Buddh Nagar,
Oraiyya, Pilibhit, Etawah, Farrukhabad,
U.P-201301.
Firozbad, Gautambodhanagar, Ghaziabad,
Tel.: 0120-2514250 / 2514252 / 2514253
Hardoi, Shahjahanpur, Hapur, Shamli, Rampur,
Kashganj, Sambhal, Amroha, Hathras,
Kanshiramnagar, Saharanpur.
PATNA -
Bihar,
Office of the Insurance Ombudsman,
Jharkhand.
1st Floor, Kalpana Arcade Building,,
Bazar Samiti Road,
Bahadurpur,
Patna 800 006.
Tel.: 0612-2680952
PUNE -
Maharashtra,
Office of the Insurance Ombudsman,
Area of Navi Mumbai and Thane
Jeevan Darshan Bldg., 3rd Floor,
excluding Mumbai Metropolitan Region.
C.T.S. No.s. 195 to 198,
N.C. Kelkar Road, Narayan Peth,
Pune - 411 030.
Tel.: 020 - 41312555
Page 18 of 25
Group Activ Travel - UIN
Annexure I - List of Day Care Surgeries
Microsurgical operations on the middle ear
1. Tympanoplasty (closure of an eardrum perforation/reconstruction of the auditory ossicles) for
tympanic membrane injury
Other operations on the middle & internal ear
2. Surgeries for Injuries on middle and inner ear
Operations on the nose & the nasal sinuses
3. Surgeries for nasal injuries
4. Nasal repair due to fracture nasal bone
5. Foreign body removal from nose
Operations on the eyes
6. Excision and destruction of diseased tissue of the eyelid
7. Removal of a foreign body from the conjunctiva
8. Removal of a foreign body from the cornea
9. Removal of a foreign body from the lens of the eye
10. Removal of a foreign body from the posterior chamber of the eye
11. Removal of a foreign body from the orbit and eyeball
12. Diathermy/Cryotherapy to treat retinal tear
13. Enucleation of Eye without Implant
14. Laser Photocoagulation to treat Retinal Tear
Operations on the skin & subcutaneous tissues
15. Surgical wound toilet (wound debridement) and removal of diseased tissue of the skin and subcutaneous
tissues
16. Local excision of diseased tissue of the skin and subcutaneous tissues
17. Simple restoration of surface continuity of the skin and subcutaneous tissues
18. Other restoration and reconstruction of the skin and subcutaneous tissues.
Operations on the tongue
19. Reconstruction of the tongue
Operations on the salivary glands & salivary ducts
20. Reconstruction of a salivary gland and a salivary duct
Other operations on the mouth & face
21. Incision, excision and destruction in the mouth
22. Palatoplasty
23. Other operations in the mouth
Operations on the female sexual organs
24. Local excision and destruction of diseased tissue of the vagina and the pouch of Douglas
Operations on the testis
25. Surgeries for testicular injury
Operations on the penis
26. Local excision and destruction of diseased tissue of the penis
Operations of bones and joints
27. Surgery for hemoarthrosis / pyoarthrosis
28. Reduction of dislocation under GA
29. Closed reduction on fracture, luxation
30. Reduction of dislocation under GA
31. Arthroscopic knee aspiration
32. Trauma surgery and orthopaedics
33. Incision on bone, septic and aseptic
34. Suture and other operations on tendons and tendon sheath
Page 19 of 25
Group Activ Travel - UIN
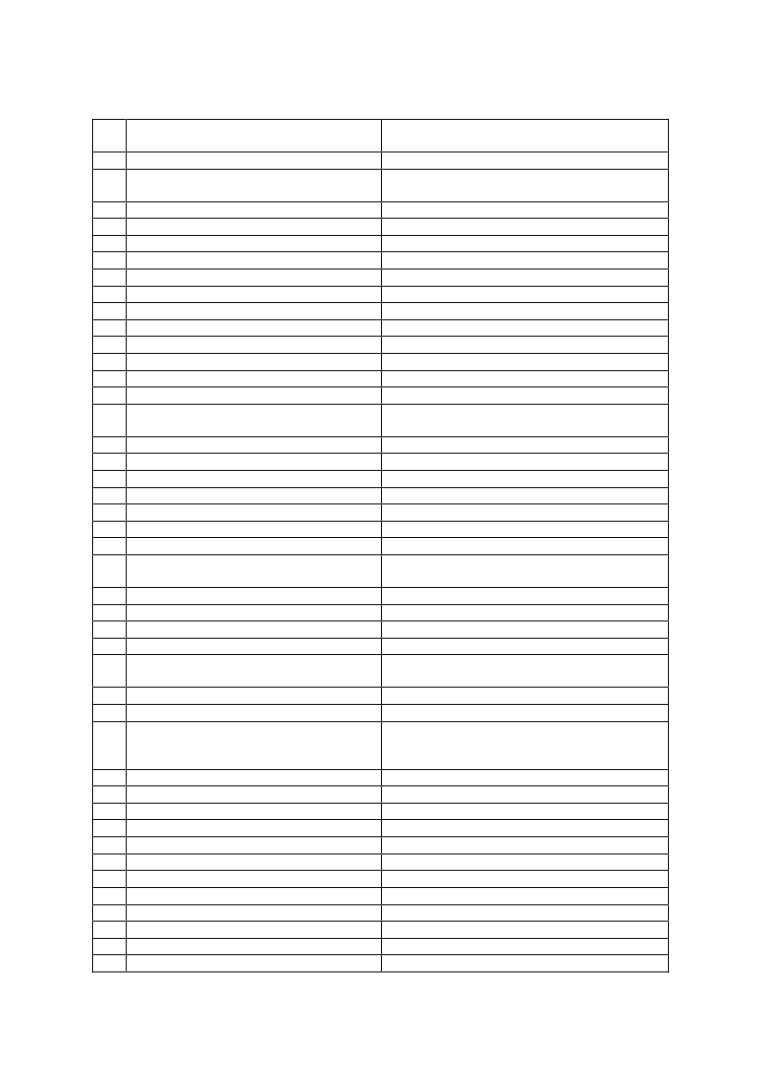
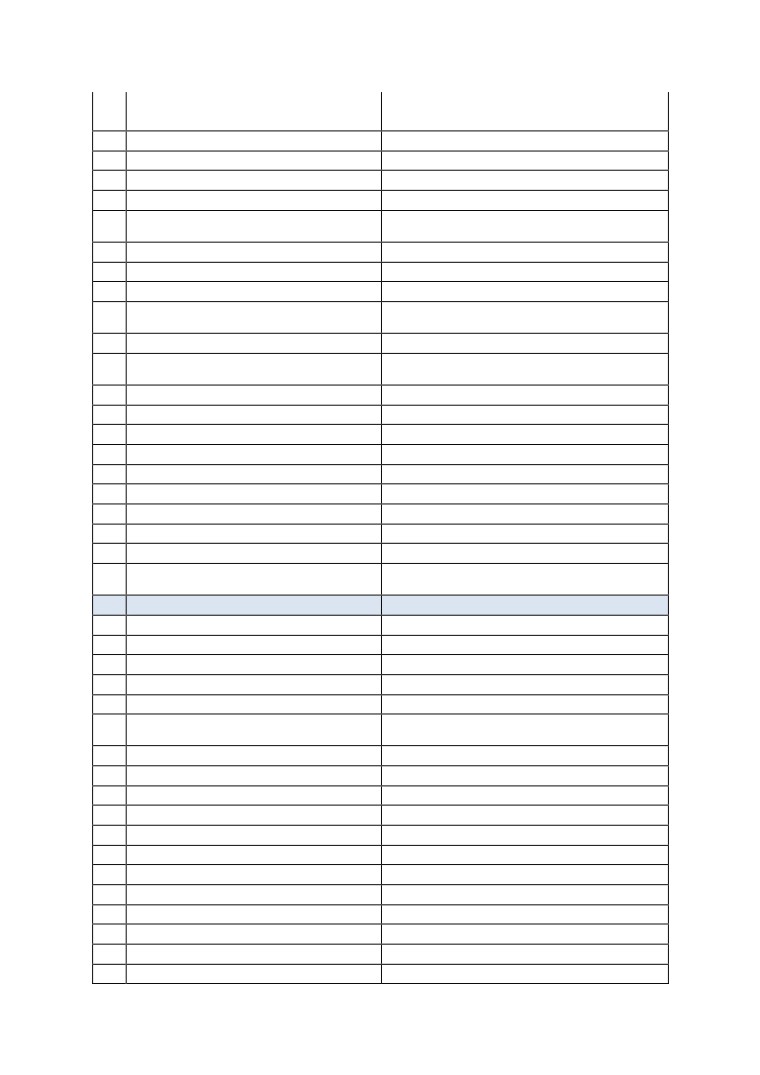
Annexure II - List of Expenses Generally Excluded “Non-Medical” Expenses
Sr.
List of Non-Medical Expenses
No.
1
HAIR REMOVAL CREAM
Not Payable
BABY CHARGES (UNLESS
2
Not Payable
SPECIFIED/INDICATED)
3
BABY FOOD
Not Payable
4
BABY UTILITES CHARGES
Not Payable
5
BABY SET
Not Payable
6
BABY BOTTLES
Not Payable
7
BRUSH
Not Payable
8
COSY TOWEL
Not Payable
9
HAND WASH
Not Payable
10
MOISTURISER PASTE BRUSH
Not Payable
11
POWDER
Not Payable
12
RAZOR
Not Payable
13
SHOE COVER
Not Payable
14
BEAUTY SERVICES
Not Payable
Essential and paid specifically for cases that have
15
BELTS/ BRACES
undergone surgery of thoracic or lumbar Spine.
16
BUDS
Not Payable
17
BARBER CHARGES
Not Payable
18
CAPS
Not Payable
19
COLD PACK/HOT PACK
Not Payable
20
CARRY BAGS
Not Payable
21
CRADLE CHARGES
Not Payable
22
COMB
Not Payable
DISPOSABLES RAZORS CHARGES ( for site
23
Payable
preparations)
24
EAU-DE-COLOGNE / ROOM FRESHNERS
Not Payable
25
EYE PAD
Not Payable
26
EYE SHEILD
Not Payable
27
EMAIL / INTERNET CHARGES
Not Payable
FOOD CHARGES (OTHER THAN PATIENT's DIET
28
Not Payable
PROVIDED BY HOSPITAL)
29
FOOT COVER
Not Payable
30
GOWN
Not Payable
Essential in bariatric and varicose vein surgery and
31
LEGGINGS
may be considered for at least these conditions
where surgery itself is payable.
32
LAUNDRY CHARGES
Not Payable
33
MINERAL WATER
Not Payable
34
OIL CHARGES
Not Payable
35
SANITARY PAD
Not Payable
36
SLIPPERS
Not Payable
37
TELEPHONE CHARGES
Not Payable
38
TISSUE PAPER
Not Payable
39
TOOTH PASTE
Not Payable
40
TOOTH BRUSH
Not Payable
41
GUEST SERVICES
Not Payable
42
BED PAN
Not Payable
43
BED UNDER PAD CHARGES
Not Payable
Page 20 of 25
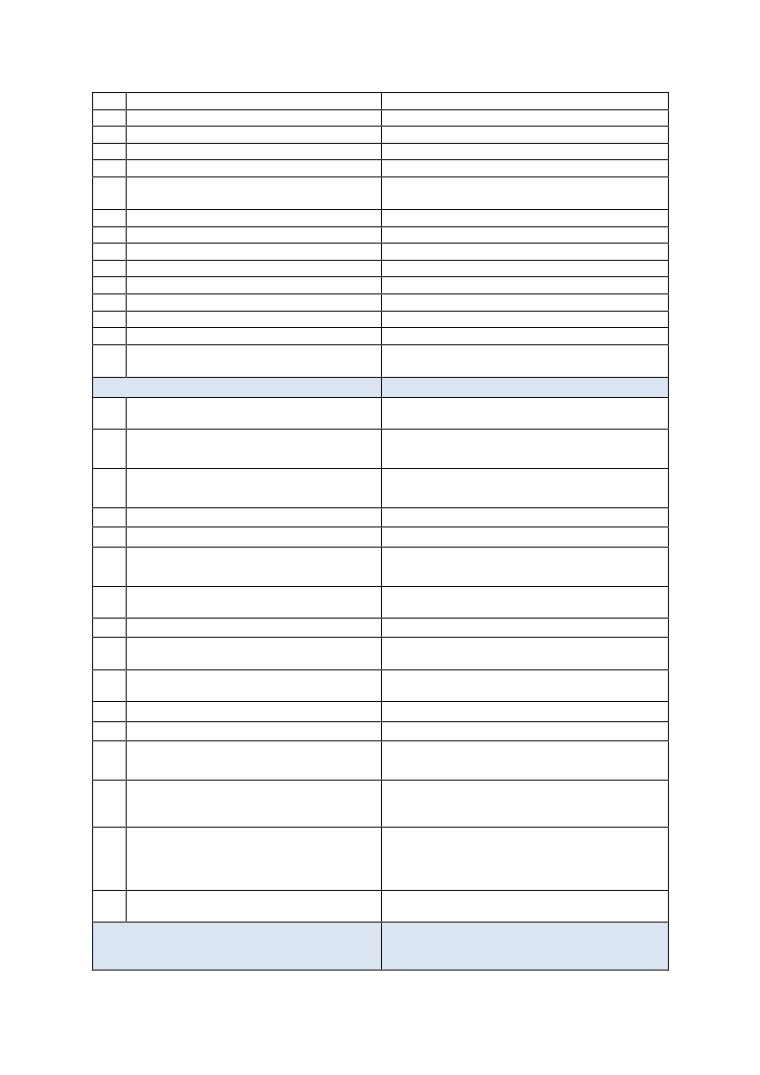
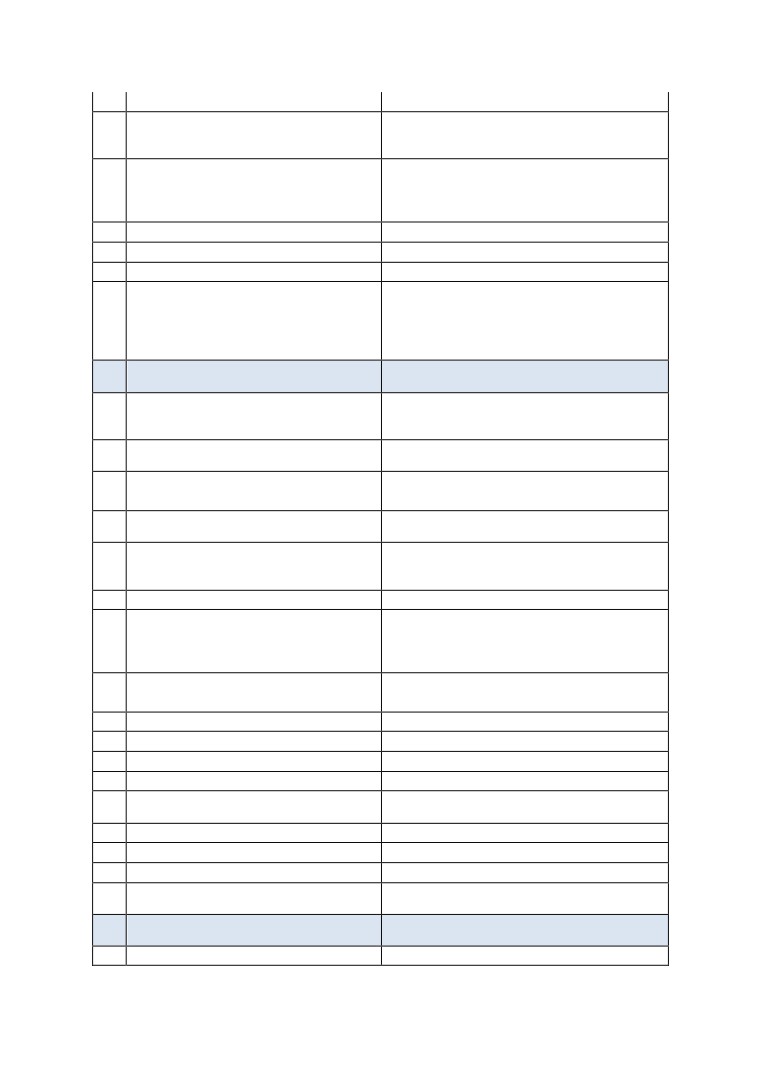
Group Activ Travel - UIN
44
CAMERA COVER
Not Payable
45
CLINIPLAST
Not Payable
46
CREPE BANDAGE
Not Payable
47
CURAPORE
Not Payable
48
DIAPER OF ANY TYPE
Not Payable
Not Payable ( However if CD is specifically sought by
49
DVD, CD CHARGES
Insurer/TPA then payable)
50
EYELET COLLAR
Not Payable
51
FACE MASK
Not Payable
52
FLEXI MASK
Not Payable
53
GAUSE SOFT
Not Payable
54
GAUZE
Not Payable
55
HAND HOLDER
Not Payable
56
HANSAPLAST/ ADHESIVE BANDAGES
Not Payable
57
LACTOGEN/ INFANT FOOD
Not Payable
Reasonable costs for one sling in case of upper arm
58
SLINGS
fractures may be considered.
ITEMS SPECIFICALLY EXCLUDED IN THE POLICIES
WEIGHT CONTROL PROGRAMS/ SUPPLIES/
59
SERVICES
Not Payable
COST OF SPECTACLES/ CONTACT LENSES/
60
HEARING AIDS ETC.,
Not Payable
DENTAL TREATMENT EXPENSES THAT DO NOT
Not Payable. (We should consider only in accident
61
REQUIRE HOSPITALISATION
cases; where Dental Surgery is required)
62
HORMONE REPLACEMENT THERAPY
Not Payable
63
HOME VISIT CHARGES
Not Payable
INFERTILITY/ SUBFERTILITY/ ASSISTED
64
CONCEPTION PROCEDURE
Not Payable
OBESITY (INCLUDING MORBID OBESITY)
65
TREATMENT
Not Payable
66
PSYCHIATRIC & PSYCHOSOMATIC DISORDERS
Not Payable
CORRECTIVE SURGERY FOR REFRACTIVE
67
ERROR
Not Payable
TREATMENT OF SEXUALLY TRANSMITTED
68
DISEASES
Not Payable
69
DONOR SCREENING CHARGES
Not Payable
70
ADMISSION/REGISTRATION CHARGES
Not Payable
HOSPITALISATION FOR EVALUATION/
71
DIAGNOSTIC PURPOSE
Not Payable
EXPENSES FOR INVESTIGATION/ TREATMENT
IRRELEVANT TO THE DISEASE FOR WHICH
72
ADMITTED OR DIAGNOSED
Not Payable
ANY EXPENSES WHEN THE PATIENT IS
DIAGNOSED WITH RETRO VIRUS + OR
SUFFERING FROM /HIV/ AIDS ETC IS
73
DETECTED/ DIRECTLY OR INDIRECTLY
Not Payable
Not Payable except Bone Marrow Transplantation
74
STEM CELL IMPLANTATION/ SURGERY
where covered by policy
ITEMS WHICH FORM PART OF HOSPITAL SERVICES
WHERE SEPARATE CONSUMABLES ARE NOT
PAYABLE BUT THE SERVICE IS
Page 21 of 25
Group Activ Travel - UIN
75
WARD AND THEATRE BOOKING CHARGES
Payable under OT Charges, not payable separately
76
ARTHROSCOPY & ENDOSCOPY INSTRUMENTS
Not Payable
77
MICROSCOPE COVER
Payable under OT Charges, not payable separately
SURGICAL BLADES,HARMONIC
78
SCALPEL,SHAVER
Not Payable
79
SURGICAL DRILL
Not Payable
80
EYE KIT
Payable under OT Charges, not payable separately
81
EYE DRAPE
Payable under OT Charges, not payable separately
Payable under Radiology Charges, not as
82
X-RAY FILM
consumable
83
SPUTUM CUP
Not Payable
84
BOYLES APPARATUS CHARGES
Payable under OT Charges, not payable separately
BLOOD GROUPING AND CROSS MATCHING OF
Not Payable
85
DONORS SAMPLES
86
ANTISEPTIC OR DISINFECTANT LOTIONS
Not Payable
BAND AIDS, BANDAGES, STERLILE INJECTIONS,
Not Payable
87
NEEDLES, SYRINGES
88
COTTON
Not Payable
89
COTTON BANDAGE
Not Payable
90
MICROPORE/ SURGICAL TAPE
Not Payable
91
BLADE
Not Payable
92
APRON
Not Payable
93
TORNIQUET
Not Payable
94
ORTHOBUNDLE, GYNAEC BUNDLE
Not Payable
95
URINE CONTAINER
Not Payable
ELEMENTS OF ROOM CHARGE
Not Payable. If there is no Policy Exclusion, then
Actual Tax Levied by Government is Payable -Part of
96
LUXURY TAX
Room Charge for Sub Limits
97
HVAC
Not Payable
98
HOUSE KEEPING CHARGES
Not Payable
SERVICE CHARGES WHERE NURSING CHARGE
99
ALSO CHARGED
Not Payable
Payable - If under room charges not if separately
100
TELEVISION & AIR CONDITIONER CHARGES
levied
101
SURCHARGES
Not Payable
102
ATTENDANT CHARGES
Not Payable
103
IM IV INJECTION CHARGES
Not Payable
104
CLEAN SHEET
Not Payable
EXTRA DIET OF PATIENT(OTHER THAN THAT
Not payable, Patient diet provided by Hospital is
105
WHICH FORMS PART OF BED CHARGE)
payable
106
BLANKET/WARMER BLANKET
Not Payable
ADMINISTRATIVE OR NON-MEDICAL
CHARGES
107
ADMISSION KIT
Not Payable
108
BIRTH CERTIFICATE
Not Payable
Page 22 of 25
Group Activ Travel - UIN
BLOOD RESERVATION CHARGES AND ANTE
109
NATAL BOOKING CHARGES
Not Payable
110
CERTIFICATE CHARGES
Not Payable
111
COURIER CHARGES
Not Payable
112
CONVENYANCE CHARGES
Not Payable
113
DIABETIC CHART CHARGES
Not Payable
DOCUMENTATION CHARGES /
114
ADMINISTRATIVE EXPENSES
Not Payable
115
DISCHARGE PROCEDURE CHARGES
Not Payable
116
DAILY CHART CHARGES
Not Payable
117
ENTRANCE PASS / VISITORS PASS CHARGES
Not Payable
EXPENSES RELATED TO PRESCRIPTION ON
Not Payable--To be Claimed by Patient Post -
118
DISCHARGE
Hospitalisation where admissible
119
FILE OPENING CHARGES
Not Payable
INCIDENTAL EXPENSES / MISC. CHARGES (NOT
120
EXPLAINED)
Not Payable
121
MEDICAL CERTIFICATE
Not Payable
122
MAINTAINANCE CHARGES
Not Payable
123
MEDICAL RECORDS
Not Payable
124
PREPARATION CHARGES
Not Payable
125
PHOTOCOPIES CHARGES
Not Payable
126
PATIENT IDENTIFICATION BAND / NAME TAG
Not Payable
127
WASHING CHARGES
Not Payable
128
MEDICINE BOX
Not Payable
129
MORTUARY CHARGES
Payable - upto 24 hrs, shifting charges not payable
MEDICO LEGAL CASE CHARGES (MLC
130
CHARGES)
Not Payable
EXTERNAL DURABLE DEVICES
Not Payable
131
WALKING AIDS CHARGES
Not Payable
132
BIPAP MACHINE
Not Payable
133
COMMODE
Not Payable
134
CPAP/ CAPD EQUIPMENTS
Not Payable
135
INFUSION PUMP - COST
Not Payable
OXYGEN CYLINDER (FOR USAGE OUTSIDE THE
136
HOSPITAL)
Not Payable
137
PULSEOXYMETER CHARGES
Not Payable
138
SPACER
Not Payable
139
SPIROMETRE
Not Payable
140
SPO2 PROBE
Not Payable
141
NEBULIZER KIT
Not Payable
142
STEAM INHALER
Not Payable
143
ARMSLING
Not Payable
144
THERMOMETER
Not Payable
145
CERVICAL COLLAR
Not Payable
146
SPLINT
Not Payable
147
DIABETIC FOOT WEAR
Not Payable
148
KNEE BRACES ( LONG/ SHORT/ HINGED)
Not Payable
Page 23 of 25
Group Activ Travel - UIN
149
KNEE IMMOBILIZER/SHOULDER IMMOBILIZER
Not Payable
Payable - If Essential and should be paid at least
specifically for cases who have undergone surgery
150
LUMBO SACRAL BELT
of lumbar spine.
Payable -for any ICU patient requiring more than 3
days in ICU, all patient with paraplegia /quadriplegia
NIMBUS BED OR WATER OR AIR BED
or for any major illness requiring prolonged
151
CHARGES
hospitalization. (Prevent Bed Sores & DVT)
152
AMBULANCE COLLAR
Not Payable
153
AMBULANCE EQUIPMENT
Not Payable
154
MICROSHEILD
Not Payable
Payable - If Essential and should be paid at least in
post surgery patients of major abdominal surgery
including TAH, LSCS, incisional hernia repair,
exploratory laparotomy for intestinal obstruction,
155
ABDOMINAL BINDER
liver transplant etc.
ITEMS PAYABLE IF SUPPORTED BY A
PRESCRIPTION
Payable when prescribed for patient, not payable
BETADINE \ HYDROGEN PEROXIDE\SPIRIT\\ \
for hospital use in OT or ward or for dressings in
156
DISINFECTANTS ETC
hospital
PRIVATE NURSES CHARGES- SPECIAL NURSING
Not Payable
157
CHARGES
NUTRITION PLANNING CHARGES - DIETICIAN
158
CHARGES / DIET CHARGES
Not Payable
Payable - Sugar free variants of admissible
159
SUGAR FREE Tablets
medicines are not excluded
CREAMS POWDERS LOTIONS (Toiletries are
not payable, only prescribed medical
160
pharmaceuticals payable)
Payable - If prescribed
161
Digestion Gels
Payable - If prescribed
Payable - Upto 5 electrodes are required for every
case visiting OT or ICU. For longer stay in ICU, may
require a change and at least one set every second
162
ECG ELECTRODES
day must be payable.
Payable -Sterilized Gloves Payable.
163
GLOVES
Unsterilized Gloves not Payable
164
HIV KIT
Payable
165
LISTERINE/ ANTISEPTIC MOUTHWASH
Payable - If prescribed
166
LOZENGES
Payable - If prescribed
167
MOUTH PAINT
Payable - If prescribed
Payable - If used during hospitalization is payable
168
NEBULISATION KIT
reasonably
169
NOVARAPID
Payable - If prescribed
170
VOLINI GEL/ ANALGESIC GEL
Payable - If prescribed
171
ZYTEE GEL
Payable - If prescribed
Routine Vaccination not Payable / Post Bite
172
VACCINATION CHARGES
Vaccination Payable
PART OF HOSPITAL'S OWN COSTS AND NOT
PAYABLE
173
AHD
Not Payable
Page 24 of 25
Group Activ Travel - UIN
174
ALCOHOL SWABES
Not Payable
175
SCRUB SOLUTION/STERILLIUM
Not Payable
OTHERS
176
VACCINE CHARGES FOR BABY
Not Payable
177
AESTHETIC TREATMENT / SURGERY
Not Payable
178
TPA CHARGES
Not Payable
179
VISCO BELT CHARGES
Not Payable
ANY KIT WITH NO DETAILS MENTIONED
[DELIVERY KIT, ORTHOKIT, RECOVERY KIT,
180
ETC]
Not Payable
181
EXAMINATION GLOVES
Not Payable
182
KIDNEY TRAY
Not Payable
183
MASK
Not Payable
184
OUNCE GLASS
Not Payable
OUTSTATION CONSULTANT'S/ SURGEON'S
185
FEES
Not payable
186
OXYGEN MASK
Not Payable
187
PAPER GLOVES
Not Payable
188
PELVIC TRACTION BELT
Not Payable
189
REFERAL DOCTOR'S FEES
Not Payable
190
ACCU CHECK (Glucometery/ Strips)
Not Payable
191
PAN CAN
Not Payable
192
SOFNET
Not Payable
193
TROLLY COVER
Not Payable
194
UROMETER, URINE JUG
Not Payable
Payable - Ambulance from home to hospital or inter
hospital shifts is payable/ RTA as specific
195
AMBULANCE
requirement is payable
Payable - If maximum of 3 in 48 hrs and then 1 in 24
196
TEGADERM / VASOFIX SAFETY
hrs
Payable - where medically necessary till a
197
URINE BAG
reasonable cost - maximum 1 per 24 hrs
198
SOFTOVAC
Not Payable
Payable - If Essential for case like CABG etc. where it
199
STOCKINGS
should be paid.
Page 25 of 25